Brief description of the technology solution and the added value it provides
Pulmonary embolism (PE) refers to the situation when a portion of a blood clot breaks off and travels through the blood stream, typically the deep venous system, passes through the right side of the heart (right atrium and right ventricle), and becomes lodged in a pulmonary artery, obstructing it.
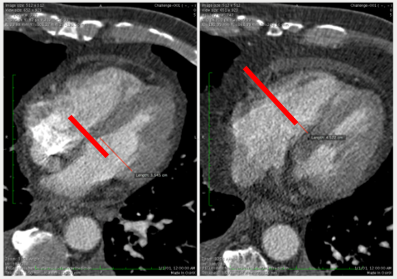
Computed tomography pulmonary angiography (CTPA) is accepted as the diagnostic imaging study of choice to confirm the clinical suspicion of acute PE. The right ventricle to left ventricle (RV/LV) diameter ratio is a proven metric of heart strain in patients with CTPA findings of acute PE.
However, such ratio is rarely done in clinical practice due to the time spent in finding the location where the diameters of the ventricles are maximal, measuring such diameters and computing the ratios. Knowledge of such metric is key to make the best medical decision for the patient.
A research team from the Technical University of Madrid, Brigham and Women’s Hospital and Massachusetts Institute of Technology, has developed a Computer Aided Diagnosis – CAD system to perform such operations automatically, without human intervention.
Description of the technological base
Quantification of RV/LV ratio can be done with several methods: volumetric measurements, four-chamber reformatted images or even in axial slices with equivalent prognostic value. Producing such measurement is time consuming and is subject to the experience of the reading radiologists.
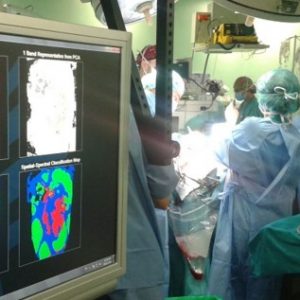
The Technical University the Madrid, together with the Brigham and Women’s Hospital and the Massachusetts Institute of Technology have designed a completely automated algorithm to compute the RV/LV axial diameter ratio. Without need for radiologists interaction, the algorithm detects the heart, segments the right and left ventricles, detects the inter-ventricular septum and finds the maximum ratio of the right ventricle with respect to the left ventricle to compute the diameter ratio. The algorithm is integrated in the Osirix radiology workstation.
The radiologist can review and correct the automated measurements before reporting them to the physician, so that he/she can make the best medical decision for the patient.
“An automated tool that will help physicians making the best medical decision for patients suffering from pulmonary embolism without incurring in extra analysis time of the images by part of the radiologists”
Market demands
-
Pulmonary embolism (PE) affects between 300,000-600,000 Americans every year and result in 12,000-80,000 deaths/year in the USA [U.S. Department of Health and Human Services, 2008].
-
Accurate numbers for Europe are scarce. However, the incidence of PE has been reported to be 6-20.8 cases/10,000 people/year in Brittany (France) and Malmo (Sweden) respectively [Torbicki et al., 2008].
-
There is an estimated number of 60,000 cases of PE a year in Spain, resulting in 50,000 hospitalizations, and more than 19,000 deaths [Juretschke Moragues & Barbosa Ayúcar, 2002] most of them without being diagnosed before death.
“James is a 75 years old patient that presents to the emergency room of the hospital with shortness of breath and chest pain. He is hemodynamically unstable. Luckily the CT scanner is available and a CTPA is performed on James. The radiology report comes and he has a saddle emboli on the pulmonary artery. The physician is faced with a doubt: shall he provide James anticoagulant therapy or is it better to perform a thrombolysis? Thankfully the report from the radiologists also included the RV/LV diameter ratio. Knowing that the RV/LV of James is 1.8, helps the physician estimate the risk of James having a heart arrest, leading to the right clinical decision”
Competitive advantages
-
Performance and robustness have been evaluated within the clinical setting on the routinely diagnostic study of PE (CTPA).
-
High accuracy when compared to measurements made by a radiologist, and prognostic significance when tested against reference standards outcomes.
-
Having an automated tool will reduce the increase of time spent by radiologists in the computation of such ratio (approximately 5 minutes/case). This will result in savings to the hospital.
-
Noise and blur artifacts typically occur in CTPA studies and the timing of the contrast can cause great differences among different CTPA scans. The key improvement of our method, with respect to algorithms designed for other cardiac CT, is the robustness with respect to these effects.
-
This tool can not only be useful in the case of acute PE, but holds promise to be used in other cardiovascular diseases, which are the leading cause of death in developed countries.
- The specific area of application is radiology. The software is integrated in the clinical setting. The system listens to events from the CT machines performing the CTPA, retrieves the associated DICOM images and performs the automated analysis in the background.
Previous references
-
Solution developed by the Technical University of Madrid, Brigham and Women’s Hospital and Massachusetts Institute of Technology.
Intellectual property
-
Provisional application for patent in USA [61/909,574]
Development stage
- Concept
- R&D
- Lab-Protoype
- Industrial Prototype
- Production
Contact
Contacto CAD
María Jesús Ledesma-Carbayo
e:
Germán González-Serrano
e:
Contacto UPM
Área de Innovación, Comercialización y Creación de Empresas
Centro de Apoyo a la Innovación Tecnológica – UPM
e: